Rational Drug Use
Probenecid & Colchicine for COVID-19 Patients
Probenecid together with colchicine(Goutyless) is often prescribed in COVID-19 cases. Although, only Colchicine is indicated in the Egyptian MOH protocol.
Also, Probenecid significantly interacts and increases the serum level of commonly prescribed medications in COVID-19 such as Meropenem and Baricitinib.
Probenecid + Meropenem —->❌Avoid combination
Probenecid + Baricitinib—-> Dose reduction for baricitinib is necessary
If the recommended dose
- 4 mg once daily, reduce the dose to 2 mg once daily.
- 2 mg once daily, reduce the dose to 1 mg once daily.
- 1 mg once daily, consider discontinuing probenecid.
Moreover, Probenecid is not preferred in renal insufficiency, which is present in many critically ill COVID-19 cases.
In conclusion, a switch to colchicine only products is recommended
Is the early use of Linezolid necessary in ICU COVID-19 cases?
Linezolid is prescribed in a number of cases, but is it really indicated in all those cases?
So when is Linezolid really indicated?
If the patient is admitted to ICU with risk factors for MRSA, including prior history of MRSA infection or colonization, recent IV antibiotics, history of recurrent skin infections or chronic wounds, presence of invasive devices, hemodialysis, recent hospital admissions, and severity of illness.
Also, it would be reasonable to perform a chest radiograph if the case is rapidly deteriorating and add linezolid if cavitating pneumonia is present.
Also, due to MAOI properties, Linezolid interacts with some anxiolytics, and anxiolytics have almost become a staple in the COVID-19 protocol.
Linezolid + Buspirone —->❌Avoid combination, high risk of serotonin syndrome.
Uncontrolled Hyperglycemia & Higher Doses of Dexamethasone
Dexamethasone is only indicated in hospitalized COVID-19 patients on supplemental oxygen or ventilatory support, and it should be administered once daily since it is a long-acting corticosteroid with a half-life of 36 to 72 hours.
The guidelines recommend a conventional dose of dexamethasone (6 mg once daily) based on the RECOVERY TRIAL, which has shown that 6 mg of dexamethasone per day for 10 days resulted in lower 28-day mortality. And the COVID STEROID-2 trial has shown that 12 mg/day hasn’t shown a statistical difference in mortality.
Trials are emerging trying to prove the efficacy and necessity of a higher dose of dexamethasone. However, there are limitations in the studies regarding diabetics, and since glucocorticoids result in uncontrolled diabetes in a dose-dependent manner. It is reasonable to follow the conventional dose (6 mg once daily) in diabetic patients.
Side Effect:
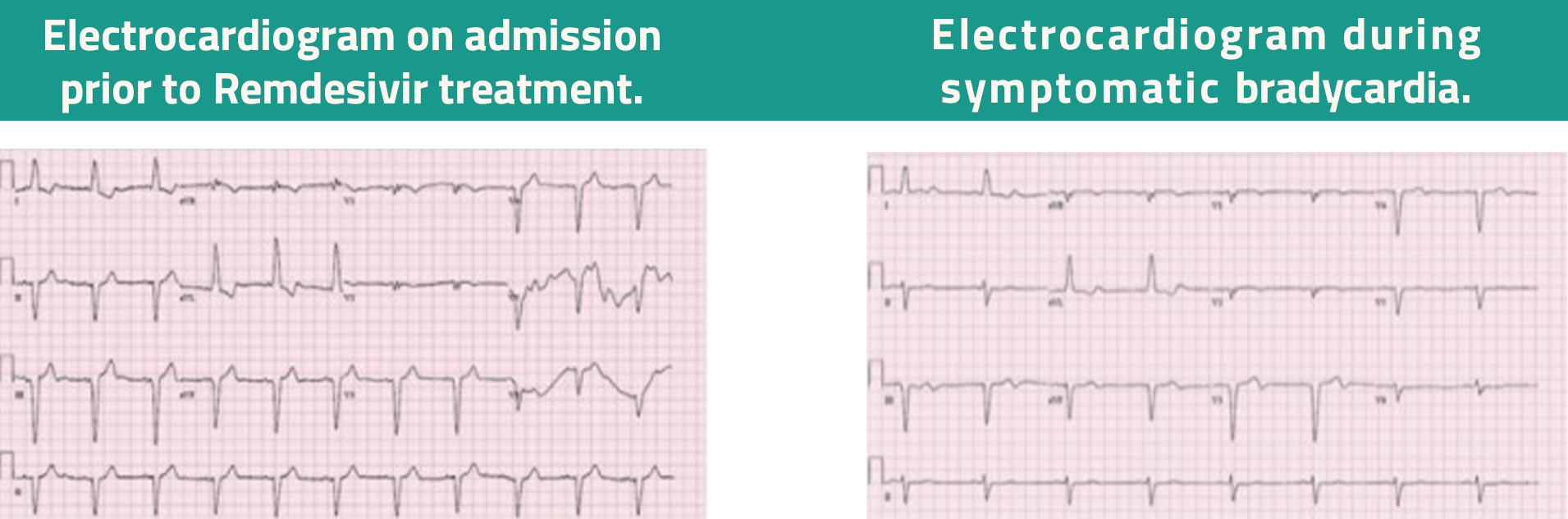
Remdesivir and Bradycardia
- Remdesivir is currently at the forefront of treatment in COVID-19 disease, given its overall results in mortality benefit and favorable safety data. The recognition of remdesivir-induced hemodynamically unstable sinus bradycardia is crucial during the treatment of COVID-19.
- Remdesivir induced bradycardia was reported in few patients – heart rate drops from 70-80s to 50s-, the effect ranges from sinus bradycardia up to severe bradycardia which is sometimes fatal. Some cases required extensive intervention as dopamine infusion to be able to complete the treatment course.
The reported average onset of this adverse event is 1 to 6 days, while other reports have noted the onset of bradycardia within 24 hours of administration of the first dose.
Physicians prefer to discontinue Remdesivir and switch to an alternative. Based on the Egyptian MOH guidelines and the patient’s criteria, Favipiravir could be an alternative.
References:
- RECOVERY TRIAL: Dexamethasone in Hospitalized Patients with Covid-19. N Engl J Med. 2021;384(8):693-704. doi:10.1056/NEJMOA2021436/SUPPL_FILE/NEJMOA2021436_DATA-SHARING.PDF
- COVID STEROID 2: https://jamanetwork.com/journals/jama/fullarticle/2785529
- https://www.thelancet.com/journals/lanres/article/PIIS2213-2600(21)00331-3/fulltext#back-bib7
- ARDS https://jamanetwork.com/journals/jama/fullarticle/2770277
- https://emcrit.org/pulmcrit/covid-steroid-2/
- Alessi J, De Oliveira GB, Schaan BD, Telo GH. Dexamethasone in the era of COVID-19: Friend or foe? An essay on the effects of dexamethasone and the potential risks of its inadvertent use in patients with diabetes. Diabetol Metab Syndr. 2020;12(1):1-11. doi:10.1186/S13098-020-00583-7/FIGURES/2
- Corticosteroids | COVID-19 Treatment Guidelines. Accessed November 10, 2021. https://www.covid19treatmentguidelines.nih.gov/therapies/immunomodulators/corticosteroids/
- Dexamethasone in the era of COVID-19: friend or foe? An essay on the effects of dexamethasone and the potential risks of its inadvertent use in patients with diabetes | Diabetology & Metabolic Syndrome | Full Text. Accessed November 16, 2021. https://dmsjournal.biomedcentral.com/articles/10.1186/s13098-020-00583-7
- https://link.springer.com/article/10.1007/s00134-021-06506-y#:~:text=Patient%2Drelated%20risk%20factors%20for,140%2C141%2C142%5D
- https://casereports.bmj.com/content/14/6/e243726
- Remdesivir-induced symptomatic bradycardia in the treatment of COVID-19 disease – ClinicalKey. Accessed November 16, 2021. https://0810fvd68-1106-y-https-www-clinicalkey-com.mplbci.ekb.eg/#!/content/journal/1-s2.0-S2214027121001007
- Remdesivir: Drug information – UpToDate. Accessed November 16, 2021. https://www.uptodate.com/contents/remdesivir-drug-information?search=remdesivir&source=panel_search_result&selectedTitle=1~29&usage_type=panel&kp_tab=drug_general&display_rank=1


